Varicose veins are often brushed off as a minor cosmetic issue, something that simply comes with age or runs in the family.
And while it’s true that they’re incredibly common (especially among women and older adults), that doesn’t mean they’re harmless.
In some cases, varicose veins are just unsightly. In others, they’re a warning sign of more serious underlying circulatory problems that shouldn’t be ignored.
So, when should you worry? And how can you tell if your veins are just a nuisance — or something your doctor needs to see?
At the Foot, Ankle & Leg Vein Center, we see these questions every day. This guide will walk you through everything you need to know, including:
- What causes varicose veins
- Early symptoms and red flags
- When varicose veins become dangerous
- At-home management strategies
- The most effective treatments available today
Whether you’ve just noticed your first bulging vein or you’ve had them for years, this article will help you understand what’s normal and what’s not.
What Are Varicose Veins?
Varicose veins are enlarged, twisted veins that typically develop in the legs due to poor blood flow. Normally, veins carry blood back to the heart using a system of one-way valves.
But when those valves weaken or fail, blood begins to pool, stretching the vein walls and causing that familiar rope-like appearance under the skin.
They can be blue, purple, or skin-colored, and they may appear raised, swollen, or twisted. Over time, the surrounding tissues may also become inflamed or tender.
Key difference from spider veins: Spider veins are smaller and closer to the surface, while varicose veins are deeper and more likely to cause discomfort.
What Causes Varicose Veins?
Several risk factors increase your chances of developing varicose veins, including:
Genetics
A family history is one of the strongest predictors. Having one parent with varicose veins increases your risk by about 40%, and if both parents have them, your risk increases to 90%.
This is because you may inherit vein structure weaknesses, faulty valves, or other circulatory traits that contribute to the condition, even if you’re otherwise healthy.
Age
Vein walls and valves naturally degrade over time. As we age, collagen and elastin (the proteins that keep blood vessels strong and flexible) start to break down.
This weakens the vein’s structure and increases the chance of malfunctioning valves, particularly in the lower legs where blood must travel furthest upward against gravity.
Prolonged Standing or Sitting
Gravity plays a major role in venous health.
Jobs that involve standing (like nurses, hairdressers, and teachers) or sitting for long hours (like drivers or office workers) lead to venous pressure buildup in the legs.
Without regular movement to help pump blood upward, the risk of valve failure and varicose vein formation increases significantly.
Pregnancy
During pregnancy, the body increases blood volume to support the growing baby, but this also means extra strain on your veins.
Hormonal shifts, particularly higher levels of progesterone, cause vein walls to relax.
Meanwhile, the uterus exerts pressure on the inferior vena cava (a major vein), which can interfere with normal blood flow from the legs.
This is why many women first develop varicose veins during pregnancy or see them worsen in subsequent pregnancies.
Obesity
Carrying excess weight adds pressure to the entire venous system, especially in the lower body.
The more pressure the veins are under, the harder it is for the valves to close properly, which leads to pooling and the development of varicose veins.
Obesity also increases inflammation, which can further damage blood vessels over time.
Lack of Physical Activity
Muscle movement is critical for healthy circulation. The calf muscles act like a pump, squeezing the veins and pushing blood upward.
A sedentary lifestyle (sitting for long periods without moving your legs) can cause blood to stagnate, weakening the veins and encouraging varicose vein formation.
Regular walking and movement are essential preventive tools.
Hormonal Changes
Estrogen has a relaxing effect on the walls of blood vessels.
Women are more prone to varicose veins partly due to hormonal factors, especially those who take birth control pills or hormone replacement therapy (HRT).
These hormonal influences can weaken vein walls over time and increase the likelihood of valve failure.
Symptoms of Varicose Veins You Shouldn’t Ignore
Varicose veins often begin as a cosmetic concern — a little bulging, some bluish discoloration, maybe a bit of swelling by the end of the day.
But as the condition progresses, symptoms can become more persistent, more painful, and more disruptive to your daily life.
Here’s what to watch for:
Aching or Heaviness in the Legs
One of the most common early symptoms. It may feel like your legs are constantly tired, especially at the end of the day or after long periods of standing.
Throbbing or Burning Sensation
Some people report a persistent “heat” or pulsing feeling near their veins, which worsens with activity or heat exposure.
Swelling in the Ankles and Lower Legs
Mild swelling that comes and goes can be a sign of venous insufficiency. If left untreated, swelling can become chronic and harder to reverse.
Restless Legs or Cramping at Night
A surprising number of patients with varicose veins experience nocturnal leg cramps or twitching, often due to poor circulation and inflammation.
Skin Changes
This is one of the more serious warning signs. Skin around the ankles and calves may darken, become dry or leathery, or develop eczema-like irritation. These are signs that blood flow is no longer adequate, and tissue health is at risk.
Itching or Burning Over a Vein
Localized discomfort can signal inflammation (phlebitis) or clot formation. If the skin is hot, red, or tender to the touch, you should see a doctor right away.
When Varicose Veins Become a Medical Problem
So, when should you stop monitoring your veins at home and actually see a doctor?
Here are signs your varicose veins may be more than just a cosmetic issue:
- Persistent swelling or pain that interferes with your daily activities
- Skin breakdown, ulcers, or open sores around the ankles
- Sudden hardening of a vein accompanied by redness and tenderness
- Bleeding from a varicose vein (even minor injuries can cause profuse bleeding in advanced cases)
- A feeling of heat, tightness, or pressure that wasn’t present before
These are signs of advanced venous insufficiency, and they require professional evaluation.
At the Foot, Ankle & Leg Vein Center, we assess not just the appearance of your veins, but the underlying health of your vascular system using tools like ultrasound diagnostics and venous reflux testing.
Left untreated, varicose veins can lead to chronic pain, skin damage, and serious complications. Early intervention makes a big difference.
Are Varicose Veins Dangerous? Potential Complications
While many people live with varicose veins without major health issues, ignoring them for too long can lead to complications, some of them serious:
Chronic Venous Insufficiency (CVI)
This is when your leg veins can no longer pump blood effectively. Symptoms include swelling, skin thickening, and ulcers. CVI can greatly affect mobility and quality of life if left unmanaged.
Superficial Thrombophlebitis
This occurs when a blood clot forms in a varicose vein close to the skin. It can cause pain, swelling, and redness, and increase the risk of deeper clot formation.
Deep Vein Thrombosis (DVT)
Though less common, untreated vein disease can sometimes progress to clots in deeper veins. DVT is a medical emergency and can lead to pulmonary embolism if the clot travels to the lungs.
Venous Ulcers
These are slow-healing open sores, typically near the ankles, caused by prolonged pressure and inflammation. They are painful, prone to infection, and very difficult to treat without medical care.
How Doctors Diagnose Vein Problems
If you’re experiencing symptoms of varicose veins, a proper diagnosis is the first step toward real relief and preventing future complications.
At the Foot, Ankle & Leg Vein Center, our doctors begin with a comprehensive vein evaluation, which may include:
Medical History and Symptom Review
We’ll ask about your lifestyle, family history, any swelling or pain, and how long your symptoms have been present.
Physical Exam
Your doctor will visually assess the veins in your legs while you’re standing. We’ll look for bulging veins, skin discoloration, swelling, or signs of inflammation.
Duplex Ultrasound
This noninvasive test uses sound waves to visualize blood flow inside the veins. It helps us detect valve malfunction, blood pooling, or hidden clots. It’s painless, fast, and highly accurate.
Venous Reflux Testing
This test checks how well your vein valves are functioning. If blood is flowing backward (reflux), it confirms chronic venous insufficiency, the underlying cause of many cases of varicose veins.
Getting an accurate diagnosis is crucial because two people with similar-looking veins may need very different treatments.
Best Treatment Options for Varicose Veins

Treatment depends on the severity of the veins, your symptoms, and whether there’s underlying venous disease. Many patients respond well to conservative therapy, while others benefit from newer, minimally invasive procedures.
Conservative Treatments
These options help relieve symptoms and slow progression:
- Compression stockings to improve circulation and reduce swelling
- Leg elevation to promote blood return
- Exercise to boost lower body circulation (walking is especially beneficial)
- Anti-inflammatory medications for pain and inflammation
Minimally Invasive Procedures
When symptoms persist or veins become painful or unsightly, we may recommend one of the following:
1. Endovenous Laser Therapy (EVLT)
A thin laser fiber is inserted into the vein, which seals it closed with heat. The body reroutes blood to healthy veins. Performed in-office under local anesthesia.
2. Radiofrequency Ablation (RFA)
Similar to EVLT, but uses radiofrequency energy. Quick recovery and little to no scarring.
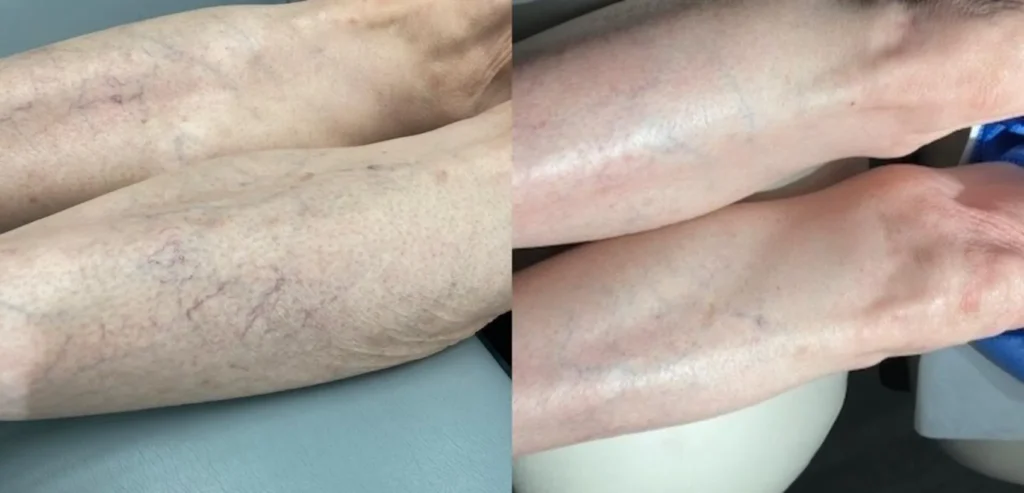
3. Sclerotherapy
A medicated solution is injected directly into the affected veins, causing them to collapse and fade over time. Ideal for smaller varicose veins and visible spider veins.
4. VenaSeal™ Closure System
A medical adhesive is used to close the diseased vein. No heat, no tumescent anesthesia, and minimal discomfort.
5. Ambulatory Phlebectomy
For larger surface veins, the vein is removed through tiny skin punctures. Often combined with EVLT or RFA for comprehensive results.
All of these procedures are performed in-office, often in under an hour, with minimal downtime.
At-Home Tips That Actually Help
While professional care is key to long-term success, there’s a lot you can do at home to reduce daily discomfort and improve your circulation:
- Walk every day — even 20 minutes helps
- Avoid sitting or standing too long without movement
- Elevate your legs for 15–20 minutes, twice daily
- Stay well hydrated and eat a low-sodium diet
- Wear graduated compression stockings consistently
- Avoid high heels and tight clothing that restrict circulation
Small changes in routine can have a big impact on how your legs feel, especially when paired with clinical treatment.
What Happens If You Ignore Varicose Veins?
Ignoring early symptoms might not seem like a big deal, but over time, vein disease tends to progress. Untreated varicose veins can lead to:
- Chronic leg pain and fatigue
- Skin damage, discoloration, and ulcers
- Blood clots and inflammation
- Reduced mobility and quality of life
The earlier you intervene, the more options you have — and the easier it is to avoid complications. Most treatments today are quick, low-risk, and done without a hospital visit.
FAQs About Varicose Veins
Can varicose veins go away on their own?
No. Once a vein has become varicose, it won’t return to normal on its own.
Conservative measures like compression stockings and exercise can reduce symptoms and slow progression, but they don’t reverse the condition.
For cosmetic or medical resolution, treatment is required.
Are men affected by varicose veins too?
Yes, although varicose veins are more common in women due to hormonal factors, men can also develop them, especially those who have a family history, are overweight, or work in jobs that require prolonged standing.
In men, symptoms are often underreported until the condition becomes painful.
Can exercise make varicose veins worse?
No, in fact, most types of low-impact exercise are beneficial. Activities like walking, swimming, and cycling help improve circulation and reduce venous pressure.
However, high-impact sports or heavy weightlifting without proper form may worsen symptoms for some individuals.
What’s the difference between treating veins for health vs. cosmetic reasons?
Health-related treatments are aimed at relieving pain, swelling, or complications like ulcers and blood clots.
Cosmetic treatments, like sclerotherapy for small surface veins, focus on appearance. However, both approaches use many of the same techniques — the key difference is why the treatment is pursued, not how it’s performed.
Take the First Step Toward Healthy Legs
If you’re wondering whether your varicose veins are more than just a cosmetic issue, you’re not alone — and you don’t have to guess.
At the Foot, Ankle & Leg Vein Center, our doctors offer expert diagnostics and personalized treatment plans tailored to your lifestyle, symptoms, and long-term vascular health. Whether you’re looking for relief, prevention, or cosmetic results, we’re here to guide you every step of the way.
Book your consultation today and find out what your veins are trying to tell you — before they demand your attention.