Healthcare providers and researchers continue to uncover the mysterious myriad of symptoms that this novel virus can cause in the wake of the COVID-19 pandemic. Coronavirus survivors and recovered COVID-19 patients are discovering that the lingering effects of COVID-19 – after the initial recovery from the virus – are far more complex and unpredictable than once thought. Leg swelling, also known as peripheral edema, is one of the unexpected post-COVID symptoms that is gaining attention.
The COVID-19 epidemic has impacted people’s lives all across the globe, and almost every day, there’s fresh information about the virus and what it causes to the body. Lately, questions have arisen about the link between COVID-19 infections, venous problems, and swollen legs after COVID-19.
Those who come down with this virus can show an array of symptoms, some of which may be mild and others that could prove severe. While cough and shortness of breath are two of the most indicative COVID-19 symptoms, it now looks like the virus could also cause swollen legs after COVID and affect veins.
The swelling has been noticed in areas throughout the body, including the hands, feet, legs, and even around the eyes. This may be the result of a number of different COVID-19 factors. For one, infection can lead to inflammation of various body areas, which can further cause fluid inside those tissues to build up. Swollen legs after COVID-19 may ensue.
Secondly, recent research has shown there might be a link between COVID-19 infection and venous thromboembolism (VTE), which is a condition in which a blood clot forms in a vein. The affected parts of the body may become sore, red, warm, or inflamed. Research suggests that people who have suffered a severe COVID-19 infection and who also dealt with specific problems caused by the virus, such as prolonged immobility or inflammation, were more likely to have blood clots and leg swelling due to COVID-19.
The critical nature of knowing how these dots connect between leg swelling, vein problems, and COVID-19 can’t be overstated — not only for professionals currently treating these symptoms but for anyone experiencing these issues as well. Recognizing these issues early allows for the best management and treatment of venous conditions that may arise during or after COVID-19 infection.
Can COVID Cause Edema in Legs?
Leg swelling, or edema, has been one of the symptoms observed in some people with the coronavirus. This symptom is usually associated with inflammation and fluid retention.
Coronavirus, which causes COVID-19, mainly affects the respiratory system but may also affect the organs and systems of other tissues of various parts of the body that contain a lot of angiotensin-converting enzyme 2 (ACE2) receptors. The ACE2 receptor belongs to the anti-inflammatory and anti-clotting arm of the renin-angiotensin system (RAS), which regulates cardiovascular health. It is through the ACE2 receptors that the coronavirus can access the cells of the human body.
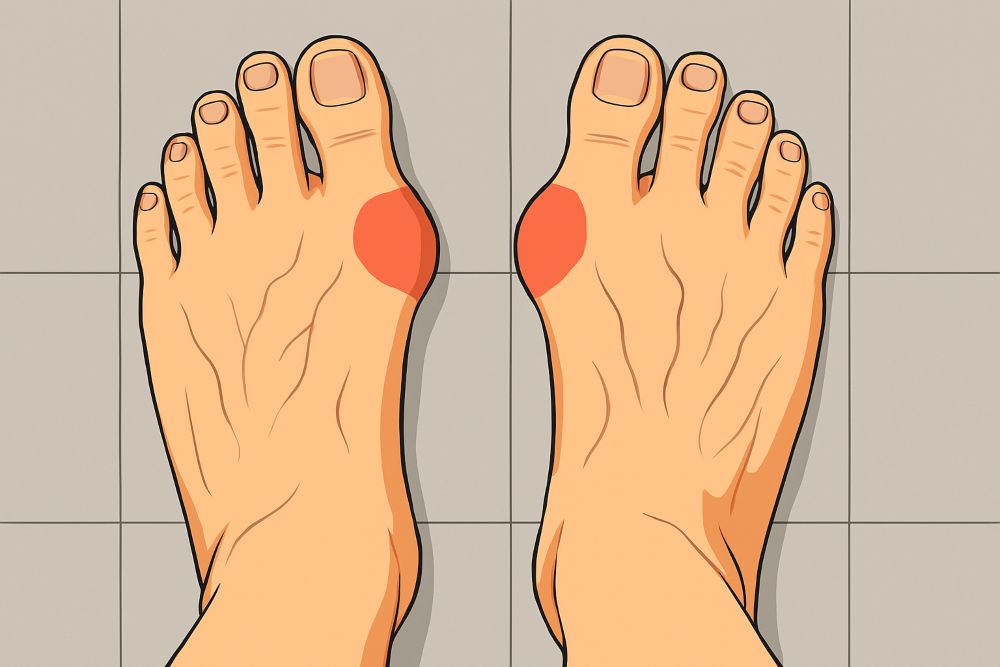
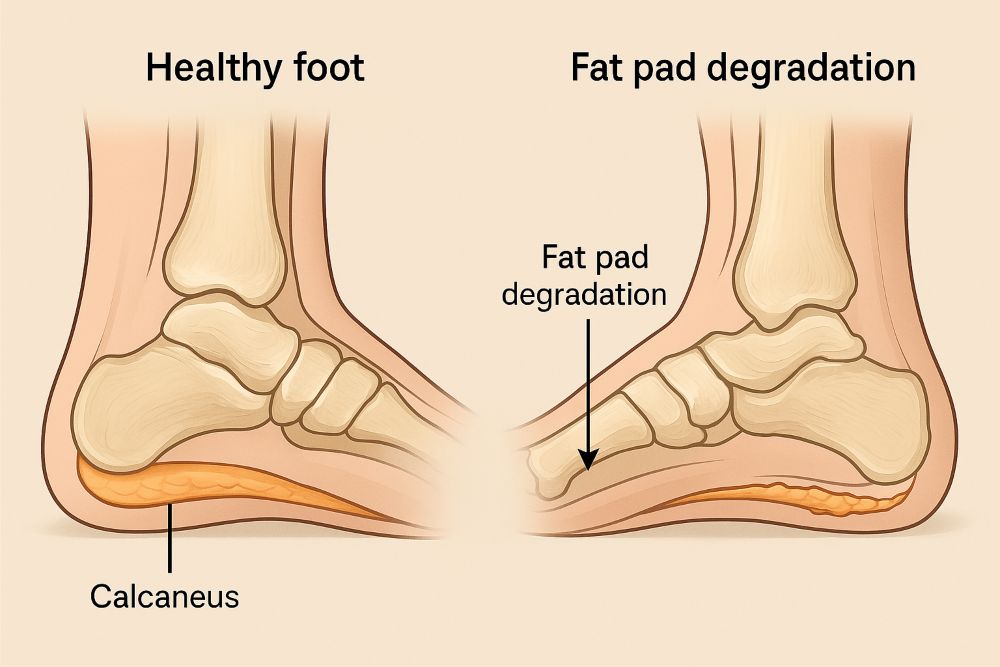
When the virus enters the lung tissue, it triggers the immune system, and inflammation occurs. Inflammation is the body’s natural protection system to combat infections, but in some cases, the immune system becomes overactive, leading to excessive inflammation. With excessive inflammation, the blood vessels start to become more leaky, and then fluid travels across and starts to leak into the tissues that surround the blood vessels, forming edema or swelling. This accumulation of fluid in the toes and fingers is known as acral edema. In acral edema, there is leg swelling and redness in the hands and feet primarily, and the affected areas can be warm and tender.
COVID has also been found to be associated with heart or kidney disease; these may cause swelling in the body as well as, in general, fluid retention. In any case, not everyone with the coronavirus experiences swelling because the severity and manifestation of symptoms differ depending on factors such as the age, overall health status, and immune response of each person.
COVID Leg Swelling and Pain
Leg pain is one reported symptom among some COVID-19 patients. The duration of this symptom will vary depending on how mild or severe the illness is. For example, in mild cases, leg pain might last for a much shorter time compared to severe cases. Again, the duration of leg pain and leg swelling in COVID-19 patients may vary from individual to individual.
Some people have leg soreness and swollen legs after COVID for a few days to a few weeks, but others will have it longer. The duration of time leg pain lingers after COVID-19 infection could also vary, as with many other symptoms. Some may see relief within a few weeks, while others may continue to feel discomfort for several months.
Leg pain and swollen legs after COVID among COVID-19 patients often come from a variety of causes. COVID-19 patients have been observed to form blood clots, among other side effects. Blood clots are due to an increased risk of clotting caused by the infection and, in severe cases, may even result in leg amputation. Inflammation causes a wide variety of additional disorders as well, which the body’s immune response is responsible for causing. This can cause swelling, redness, and pain not only in the legs but also in multiple regions.
The immune system generates infection-fighting inflammation during COVID-19. Signaling molecules that control inflammation, called cytokines, are produced during the immunological response. However, an excessively strong or prolonged immune response might cause chronic muscle pain and swelling.
Blood Clotting and Deep Vein Thrombosis (DVT)
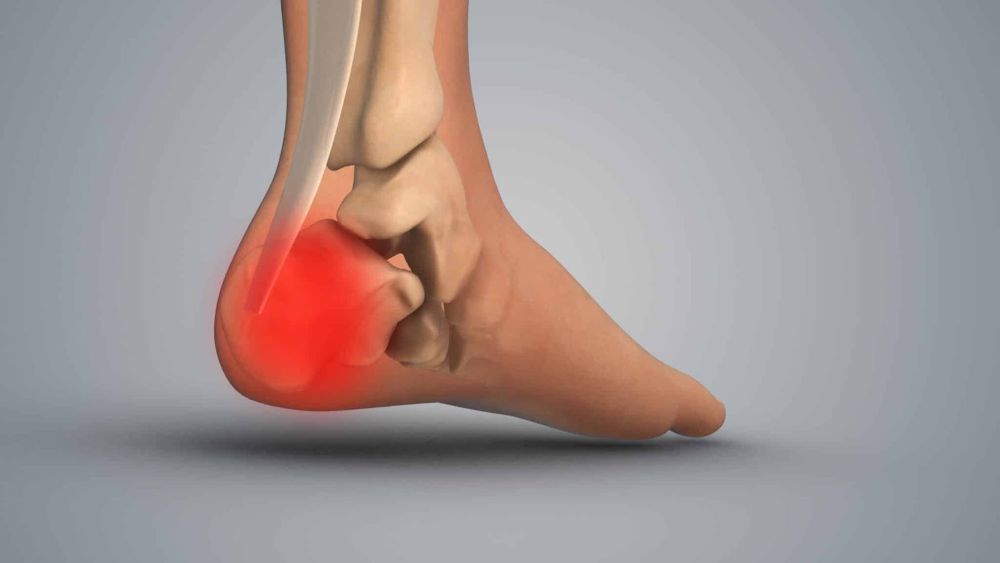
Deep vein thrombosis (DVT) is brought on by blood clots in the deep veins, typically in the legs. Concerns have been raised during the pandemic by reports that COVID-19 patients are more likely to develop DVT.
Regarding DVT and COVID-19, a few findings have been drawn. For example, it can show up in individuals who don’t show the classic signs and symptoms of a blood clot. DVT typically causes the affected limb to be painful, grow warm, redden, and have leg swelling. Furthermore, symptoms can differ from person to person.
DVT treatment objectives usually seek to avert the formation of additional clots and lessen the possibility of complications. Doctors may prescribe anticoagulant medications to reach those goals. More aggressive treatments, such as thrombolytic therapy or surgical procedures, could be called for in more severe instances or when complications are anticipated.
COVID-19 Medications and Worsening Vein Conditions
Some of the antiviral medications being used to treat COVID-19 may have venous side effects, according to recent research. As these medicines increase blood clotting, which is an existing problem, they also increase preexisting venous issues. Some antiviral drugs used to treat COVID can also increase the risk of blood clots. Healthcare professionals need to constantly watch out for venous problems in patients using COVID-19 medications.
People with vein problems, such as varicose veins or DVT (deep vein thrombosis), maybe more impacted by some of these COVID-19 treatments. Patients need to tell their doctor about their complete medical history so they can get the best treatment for COVID-19 and avoid any risks and complications.
Long COVID and Its Impact on Leg Pain and Swelling
Many persons with long-term COVID-19, also known as post-acute sequelae of SARS-CoV-2 infection, continue to have symptoms even after they have recovered from the virus. One of the most prevalent complaints among long-term COVID-19 patients is recurrent leg discomfort.
Leg swelling and pain due to COVID can involve a variety of sensations, like cramping and muscle aching. Often, these people need to take some rest to do activities of daily living, such as walking, standing for an extended period, or exercising.
The leg pain associated with long-term COVID patients often comes with a significant decrease in muscle strength or a type of muscle weakness that makes movement difficult. It may be in one or both legs and get better or worse throughout the day.
The leg pain and swelling found among long COVID patients may be due to a number of conditions. Aside from blood clots and inflammation, there could also be peripheral arterial disease, pulmonary embolism, or even nerve damage. Covid-19 can produce nerve damage throughout the body, which could result in peripheral neuropathy, which would further cause pain and numbness in the legs.
Leg Swelling and Pain Due to COVID-19 Vaccination
One journal report described temporary lower extremity lymphedema after SARS-CoV-2 vaccination. Lymphedema takes place when fluid lymph accumulates in tissues, causing pain and swelling. It is presumed an immunologic response is the etiology despite the fact that the pathophysiology is not known.
Some cases of temporary lower extremity lymphedema associated with COVID vaccinations have been reported and are predominantly connected to immunizations with mRNA-based vaccines, for example, Moderna (mRNA-1273) and BioNTech BNT162b2. The swelling often affects one or both legs days to weeks after vaccination and spontaneously subsides days to weeks after vaccination. However, these cases are rare.
Tips for Leg Pain and Swelling: When to Seek Medical Help
Whether you are still suffering from COVID or have already recovered, it’s always beneficial to follow specific tips to avoid leg pain and swollen legs after COVID and improve overall cardiovascular health. This may involve regular leg elevation, ensuring adequate electrolyte intake, frequently exercising, and using compression stockings to minimize fluid retention.
Consuming a diet rich in nutrients that decrease inflammation is also advised. Inflammation-busting foods such as leafy greens and fatty fish (like salmon or tuna) are rich in antioxidants and can help promote vein health. Turmeric, such as in curry dishes and almonds, can also help boost cardiovascular health.
There are also breathing techniques that can help to lower inflammation and yoga moves that can improve venous return and prevent swollen legs after COVID-19.
For those COVID patients who are affected with mild leg pain and swelling, analgesics such as acetaminophen, aspirin, and ibuprofen may help. These pain-relievers are temporary and don’t deal with the actual cause of the leg pain and swelling.
Seek the advice of a physician when you have leg pain and swelling due to COVID-19 or other medical conditions. Severe, rapid swelling in the legs or any other part of your body could indicate an underlying condition such as deep vein thrombosis or venous insufficiency. Contact a physician if you notice swollen legs after COVID-19 or experience pain, warmth, redness, and discomfort.
Also, see a doctor if your family has a history of clotting disorders or if you have had blood clots before. Having difficulty breathing or walking indicates a more serious medical problem that needs emergency medical attention right away.
Final Thoughts
Understanding the extent of leg swelling and pain during and after COVID-19 infection is critical for physicians and other healthcare professionals. Angiotensin peptides cause blood clotting, inflammation, and other vascular issues. Healthcare professionals should consider every patient with leg pain and swelling as a potential COVID-19 patient. By being aware of potential risks, healthcare professionals can provide the most effective care strategies, help patients maintain a healthy lifestyle, and help them seek medical attention for any of the above-mentioned symptoms.
References
- Carpenter RM, Young MK, Petri WAO, Lyons GR, Gilchrist C, Carey RM, Petri WA Jr. Repressed Ang 1-7 in COVID-19 Is Inversely Associated with Inflammation and Coagulation. mSphere. 2022 Aug 31;7(4):e0022022. doi: 10.1128/msphere.00220-22. Epub 2022 Aug 1. PMID: 35913134; PMCID: PMC9429950. https://pubmed.ncbi.nlm.nih.gov/35913134/
- Chen L, Deng H, Cui H, Fang J, Zuo Z, Deng J, Li Y, Wang X, Zhao L. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget. 2017 Dec 14;9(6):7204-7218. doi: 10.18632/oncotarget.23208. PMID: 29467962; PMCID: PMC5805548.
- Chippa V, Aleem A, Anjum F. Post-Acute Coronavirus (COVID-19) Syndrome. [Updated 2023 Feb 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK570608/
- Chung JH, Sohn SM, Yoo HJ, Yoon ES, Park SH. Transient lower extremity lymphedema following COVID-19 vaccination: A case report. Medicine (Baltimore). 2021 Dec 3;100(48):e28092. doi: 10.1097/MD.0000000000028092. PMID: 35049235; PMCID: PMC9191610.
- Gerotziafas GT, Catalano M, Colgan MP, Pecsvarady Z, Wautrecht JC et al. Guidance for the Management of Patients with Vascular Disease or Cardiovascular Risk Factors and COVID-19: Position Paper from VAS-European Independent Foundation in Angiology/Vascular Medicine. Thromb Haemost. 2020 Dec;120(12):1597-1628. doi: 10.1055/s-0040-1715798. Epub 2020 Sep 13. PMID: 32920811; PMCID: PMC7869052.
- Jain U. Effect of COVID-19 on the Organs. Cureus. 2020 Aug 3;12(8):e9540. doi: 10.7759/cureus.9540. PMID: 32905500; PMCID: PMC7470660.
- Razi M, Gu J, He X, Kong J, Ahmed MJ. Venous thromboembolism in patients with COVID-19. A prevalent and a preventable complication of the pandemic. J Interv Med. 2021 May;4(2):62-65. doi: 10.1016/j.jimed.2021.02.006. Epub 2021 Feb 26. PMID: 34557323; PMCID: PMC7908849.
- Valtueña J, Ruiz-Sánchez D, Volo V, Manchado-López P, Garayar-Cantero M. Acral edema during the COVID-19 pandemic. Int J Dermatol. 2020 Sep;59(9):1155-1157. doi: 10.1111/ijd.15025. Epub 2020 Jul 1. PMID: 32608503; PMCID: PMC7361594.
- Widyadharma IPE, Sari NNSP, Pradnyaswari KE, Yuwana KT, Adikarya IPGD et al. Pain as clinical manifestations of COVID-19 infection and its management in the pandemic era: a literature review. Egypt J Neurol Psychiatr Neurosurg. 2020;56(1):121. doi: 10.1186/s41983-020-00258-0. Epub 2020 Dec 27. PMID: 33390724; PMCID: PMC7767578.