You wake up in the morning, step out of bed, and feel that stabbing pain in your heel. It might ease up after a few steps, or maybe it lingers all day, making every movement a reminder that something’s not right.
Two of the most common culprits are heel spurs and plantar fasciitis.
And while the symptoms often overlap, these conditions are not the same, and treating them as if they are can lead to frustration, delays in healing, or unnecessary procedures.
So, how can you tell the difference? In this guide, we’ll explain:
- What heel spurs and plantar fasciitis really are
- How to recognize the signs of each
- When to seek treatment
- And how to finally get long-term relief
At the Foot, Ankle & Leg Vein Center, we help patients every day who are struggling with heel pain and are unsure of what’s really causing it.
Whether you’re dealing with symptoms yourself or trying to support someone who is, this article will help you understand the key differences and what to do next.
What Is a Heel Spur?
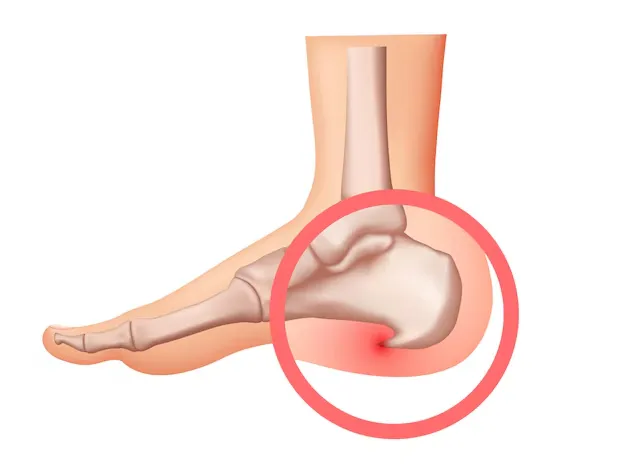
A heel spur is a calcium deposit that builds up over time on the underside of the heel bone.
It forms where the plantar fascia ligament attaches to the heel, and over months or years of stress, inflammation, or tension, a small bony growth may develop.
But here’s the catch: heel spurs themselves don’t always cause pain. Many people have them and don’t even know it.
In fact, heel spurs are often found on X-rays done for other reasons. When pain does occur, it’s usually because of inflammation in the surrounding tissue, not the spur itself digging into anything.
Common characteristics of heel spurs:
- Sharp pain with the first steps in the morning
- Pain that improves slightly with movement
- A dull ache after prolonged standing or walking
- Often discovered incidentally on an X-ray
What Is Plantar Fasciitis?
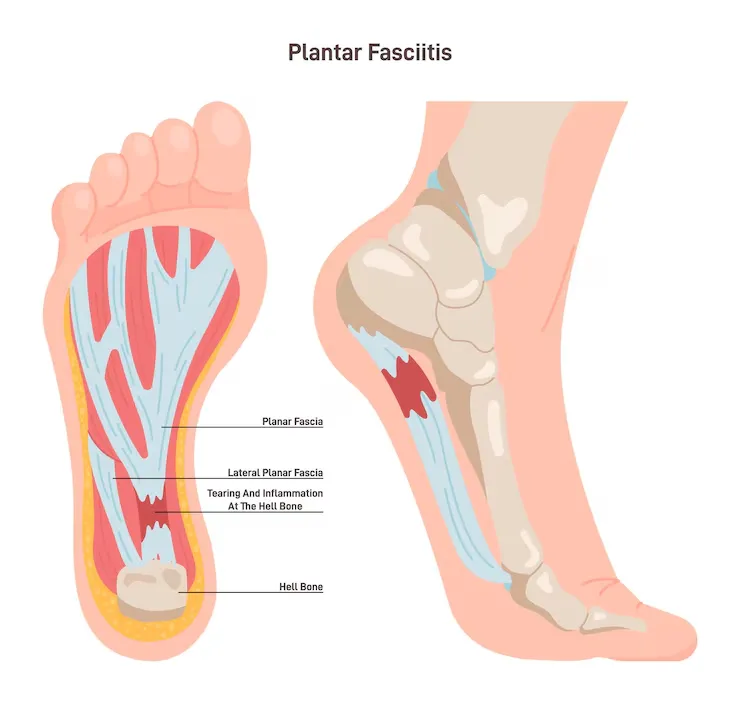
Plantar fasciitis is one of the most common causes of heel pain in adults.
It’s an inflammation of the plantar fascia, the thick band of tissue that runs along the bottom of your foot, connecting the heel bone to the toes.
Unlike heel spurs, plantar fasciitis is a soft tissue condition, and the pain comes from tiny micro-tears in the ligament itself, usually due to overuse, poor biomechanics, or lack of support.
Key signs of plantar fasciitis:
- Stabbing pain in the heel when first getting out of bed
- Pain after long periods of rest (like driving or sitting at a desk)
- Tenderness in the arch of the foot
- Pain triggered by walking barefoot on hard surfaces
How Are Heel Spurs and Plantar Fasciitis Different?
Although heel spurs and plantar fasciitis are closely related, and sometimes even occur together, they are distinct conditions with different causes, diagnostic methods, and treatment approaches.
The core difference is this:
- A heel spur is a bone growth.
- Plantar fasciitis is an inflammation of the ligament.
Pain from a heel spur is often more localized to the bottom of the heel bone, especially if the spur irritates nearby soft tissues.
With plantar fasciitis, the pain tends to radiate from the heel into the arch of the foot and can be aggravated by poor footwear, tight calves, or overuse.
Diagnostic process:
- Plantar fasciitis is diagnosed based on symptoms and physical exam.
- Heel spurs are confirmed via X-ray imaging, though not all require treatment.
Understanding which condition is present is critical. Why? Because treatment for one may not help the other.
Stretching, for example, can do wonders for plantar fasciitis, but may not relieve pain from an inflamed spur pressing into tissue.
Can You Have Both at the Same Time?
Yes, and many people do.
In fact, up to 50% of people with plantar fasciitis also develop a heel spur.
That’s because both conditions can stem from the same root causes:
- Tight or overused plantar fascia
- Repetitive stress on the heel bone
- Poor foot mechanics
- Long hours on hard surfaces
Having both doesn’t necessarily make symptoms worse, but it does make accurate diagnosis and individualized treatment even more important.
At Foot, Ankle & Leg Vein Center, our doctors often use a combination of clinical exam and imaging to determine whether the pain is soft tissue-related, bone-related, or both, then tailor treatment accordingly.
What Causes Heel Spurs and Plantar Fasciitis?
While both conditions affect the heel, they don’t always share the same origin.
Causes of Heel Spurs:
- Chronic stress and pulling on the heel bone
- Long-term strain from flat feet or high arches
- Improper footwear
- Repetitive impact (running, jumping, prolonged standing)
Causes of Plantar Fasciitis:
- Overuse of the plantar fascia ligament
- Poor foot mechanics (e.g., flat feet, tight calves)
- Sudden increase in activity or training
- Standing or walking on hard surfaces for long periods
Understanding the cause helps guide not just treatment, but prevention.
Symptoms Comparison: Heel Spur vs. Plantar Fasciitis
The pain may feel similar, but the location and triggers often differ.
| Symptom | Heel Spur | Plantar Fasciitis |
| Morning pain | Sharp at first step, may ease quickly | Sharp or stabbing, often lingers |
| Pain location | Directly under the heel bone | Under the heel, extending into the arch |
| Pain after rest | Common | Very common |
| Visible on X-ray | Yes | No |
| Triggered by activity | Standing, walking, running | Especially walking after rest |
Best Treatment Options for Heel Pain

Whether you’re dealing with plantar fasciitis, a heel spur, or both, the good news is that most cases respond well to conservative care. Surgery is rarely needed and typically reserved for chronic, nonresponsive pain.
Here’s how treatment typically breaks down:
1. Stretching and Strengthening
- Targeting the plantar fascia and calf muscles to reduce tension
- Helps realign foot mechanics and relieve strain
- Often paired with physical therapy for long-term improvement
2. Custom Orthotics
- Redistribute pressure away from the heel and arch
- Address structural issues like flat feet or high arches
At Foot, Ankle & Leg Vein Center, our doctors fit custom orthotics based on your foot’s exact needs, not just off-the-shelf inserts
3. Supportive Footwear
- Avoid flat shoes, flip-flops, or worn-out sneakers
- Use footwear with firm heel support and proper arch contour
4. Ice and Anti-Inflammatories
- Ice therapy helps reduce swelling
- NSAIDs like ibuprofen can offer temporary relief during flare-ups
5. Cortisone Injections (if needed)
- Used cautiously for persistent inflammation
- Especially effective for plantar fasciitis that hasn’t responded to other methods
6. Advanced Treatments
For stubborn cases, options like shockwave therapy, MLS laser therapy, or platelet-rich plasma (PRP) may be recommended to stimulate healing in chronic soft tissue injuries.
Still not sure what’s causing your heel pain? Our team at Foot, Ankle & Leg Vein Center can help you find the root cause and create a personalized plan that gets you back on your feet, pain-free.
Tips for Preventing Heel Spurs and Plantar Fasciitis
While not all causes of heel pain can be prevented, especially if genetics or your profession play a role, there are smart habits that can greatly reduce your risk or prevent recurrence after treatment.
Foot-Friendly Prevention Strategies:
- Wear the right shoes.
Choose footwear with good arch support, a cushioned heel, and a firm sole. Avoid walking barefoot on hard surfaces, especially at home. - Replace worn-out shoes.
Old running or walking shoes lose support over time. If you’re active, replace your shoes every 300–500 miles or when the soles feel flat. - Stretch regularly.
Focus on the calves, Achilles tendon, and the bottom of your feet. Morning stretches are especially helpful for preventing that “first step” pain. - Don’t ignore tightness.
Tight calves and hamstrings can increase strain on the plantar fascia. Keep your lower body flexible, especially if you sit or stand for long periods. - Use custom orthotics if needed.
If you have flat feet, high arches, or other biomechanical imbalances, professionally made orthotics can make a huge difference in both prevention and recovery. - Ease into new activities.
If you’re starting a new workout or increasing your mileage, do it gradually to avoid overstressing the feet.
At Foot, Ankle & Leg Vein Center, our team doesn’t just treat heel pain; we help you build a foundation for long-term foot health.
Can You Diagnose Heel Spurs Without an X-ray?
In short: not reliably.
Plantar fasciitis is usually diagnosed through physical examination, based on symptoms, palpation, and medical history.
Heel spurs, however, are only visible through imaging. That’s why X-rays are often ordered when heel pain persists beyond a few weeks or if plantar fasciitis isn’t responding to treatment.
Do Heel Spurs Always Require Surgery?
Absolutely not. Most heel spurs can be treated conservatively, especially when pain is caused by inflammation, not the bone growth itself.
Surgery is considered only when:
- Pain is chronic and disabling
- Other treatments have failed over 6–12 months
- A large bone spur irritates soft tissues or nerves
If surgery is recommended, it’s often done in combination with plantar fascia release to relieve tension across the ligament.
What’s the Role of Footwear in Managing Heel Pain?
Shoes play a massive role in both causing and resolving heel pain.
Look for:
- Firm arch support
- Deep heel cup
- Shock-absorbing sole
Wide toe box
Avoid:
- Thin-soled sandals or flip-flops
- Flat ballet flats
- Worn-out running shoes
- High heels that shift weight forward
Is Walking Good or Bad for Plantar Fasciitis?
It depends.
Walking short distances on supportive surfaces and with the right shoes can help keep the fascia mobile and prevent stiffness.
But walking barefoot or in unsupportive footwear on hard floors often worsens symptoms.
A common mistake patients make is resting too much, which can cause the fascia to tighten. The key is gentle, supported movement, combined with stretching and footwear protection.
Can Custom Orthotics Help Heel Spurs and Plantar Fasciitis?
Yes! Especially when tailored to your biomechanics.
Custom orthotics:
- Support the arch, reducing pull on the plantar fascia
- Redistribute pressure away from the heel
- Correct gait imbalances that contribute to chronic strain
How Long Does It Take to Heal?
Recovery depends on the severity of the condition and how early treatment begins:
- Plantar fasciitis: Most cases improve within 6–12 weeks with proper care.
- Heel spurs: If symptomatic, expect 3–6 months of conservative management.
- Chronic cases may take longer and require a more structured rehab plan.
Early intervention leads to better outcomes. Delaying care can result in chronic pain or compensatory issues (like knee, hip, or back pain).
Are There Advanced Treatment Options for Chronic Heel Pain?
Yes! For persistent cases, several advanced, non-surgical options may be used:
- Extracorporeal Shockwave Therapy (ESWT): Stimulates healing by increasing blood flow and breaking down scar tissue.
- MLS Laser Therapy: Reduces inflammation and speeds tissue repair.
- Platelet-Rich Plasma (PRP): Uses your own growth factors to promote tissue regeneration.
- Dry Needling: Targets myofascial pain and chronic tension around the heel and arch.
These are available through podiatric specialists and often paired with conservative therapies for the best results.
When to See a Doctor About Heel Pain
It’s easy to ignore heel pain at first, but when it starts affecting your daily routine, it’s time to take it seriously.
You should see a foot and ankle specialist if:
- The pain lasts more than 2 weeks without improvement
- It’s worse in the morning or after rest
- You’re starting to limp or change your gait
- You’ve tried rest, ice, and better shoes, and nothing’s working
Heel pain that doesn’t go away on its own deserves a proper evaluation.
The sooner you get an accurate diagnosis, the faster you can get back to walking, working, and living without discomfort.
Heel Pain Doesn’t Have to Be Permanent
Whether it’s a heel spur, plantar fasciitis, or both, the pain you’re feeling isn’t something you have to live with.
Most cases improve with the right combination of conservative care, proper footwear, and personalized treatment.
At Foot, Ankle & Leg Vein Center, our doctors use evidence-based techniques and diagnostic tools to pinpoint the cause of your pain and build a plan that fits your life, not just your symptoms.
Schedule a consultation today and let’s take the first step toward lasting heel relief.








